Understanding the Research Gap in Musculoskeletal Care
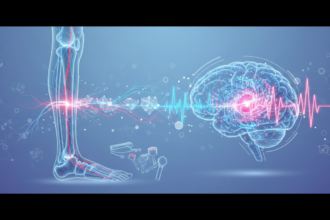
In the evolving landscape of orthopedic medicine, a persistent question remains: why do promising interventions often yield modest results in the real world? A recent study by Remis and colleagues from Duke University, titled “Why are treatment effects so small in musculoskeletal interventions? Part II: variability in clinical translation,” offers a sophisticated analysis of this phenomenon. Published in the Journal of Manual & Manipulative Therapy, this research delves into the complexities of moving evidence-based treatments from controlled research settings into the diverse and often unpredictable environment of clinical practice.
Study Overview
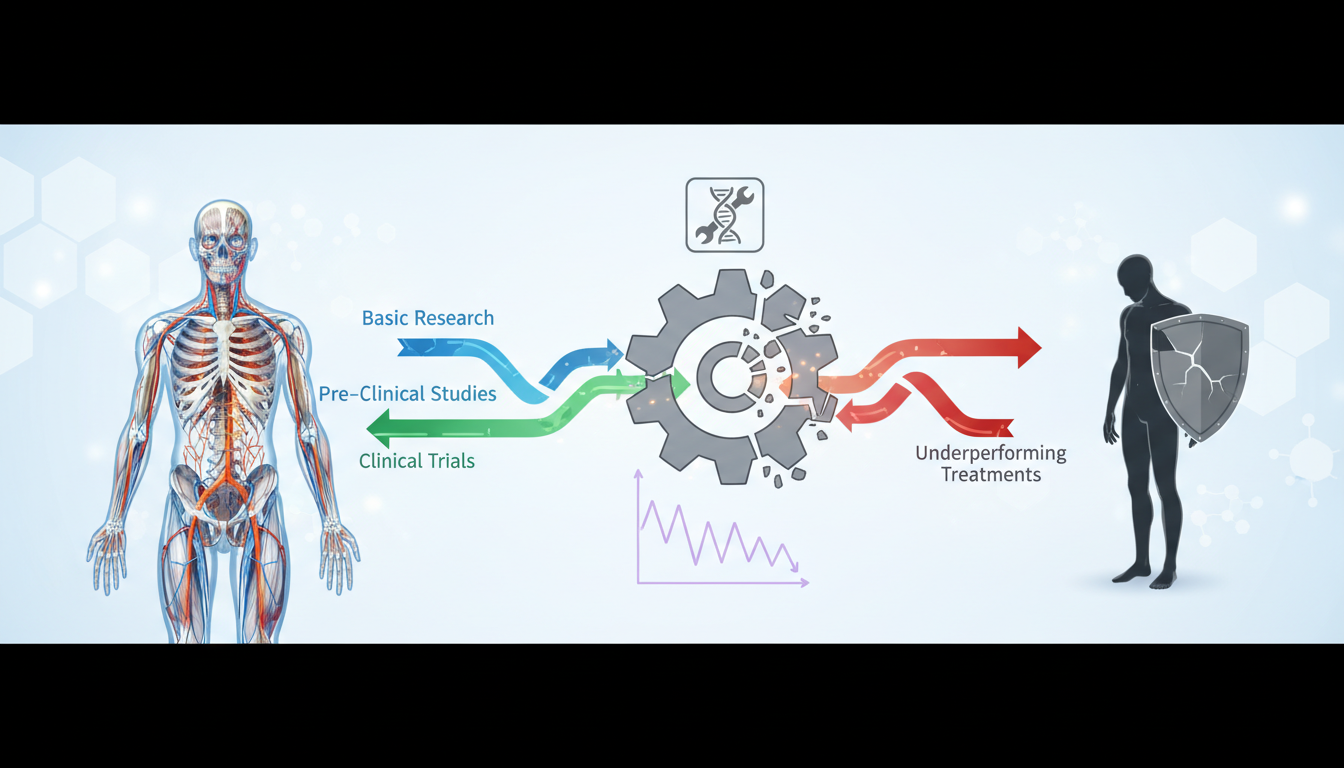
The research team, comprised of specialists from the Department of Rehabilitation Services at Duke University Health System and the Duke Clinical Research Institute, focused specifically on the concept of ‘clinical translation.’ This refers to the multifaceted process by which a standardized intervention is adapted and applied to individual patients. The study highlights that the perceived “small effects” frequently cited in musculoskeletal (MSK) research may not necessarily indicate the failure of a treatment modality itself, but rather a significant loss of efficacy during the translational phase from bench to bedside.
The Factors Influencing Clinical Translation
The researchers identified several critical areas where variability undermines treatment outcomes in the clinical setting. These factors contribute to the dilution of effect sizes seen in large-scale trials:
- Patient Heterogeneity: Real-world patients often present with multiple comorbidities and complex psychosocial factors that are frequently excluded from strictly controlled clinical trial populations.
- Therapist Variability: Differences in skill levels, educational backgrounds, and adherence to specific protocols among clinicians can lead to inconsistent delivery of the intervention.
- Environmental Context: The setting in which therapy is delivered, including time constraints, institutional culture, and reimbursement models, significantly impacts the quality of care.
- Dosage and Adherence: The translation from a fixed trial dosage to a flexible clinical schedule often results in sub-therapeutic exposure for the patient.
Clinical Findings and Implications
The core finding of this analysis is that the “noise” inherent in clinical translation often drowns out the therapeutic signal. When an intervention is applied inconsistently across different practitioners and patient types, the statistical effect size inevitably diminishes. This suggests that the musculoskeletal field requires a paradigm shift. Rather than searching for a universal ‘silver bullet’ treatment, researchers and clinicians must focus on optimizing the fidelity and delivery of existing interventions within the clinical ecosystem. Furthermore, the study posits that personalized medicine could mitigate some of these translational issues. By tailoring interventions to the specific phenotypes of patients, clinicians may reduce the negative impact of heterogeneity. However, this requires robust diagnostic tools and a deep understanding of the mechanisms behind specific treatments to ensure the right treatment reaches the right patient at the right time.
Conclusion
As we move forward in musculoskeletal rehabilitation, the insights provided by the Duke University team are invaluable. Addressing the variability in clinical translation is not just a theoretical concern; it is a practical necessity for improving patient outcomes across the board. By bridging the gap between research protocols and real-world application, the healthcare community can better realize the potential of musculoskeletal interventions. This involves improving practitioner training, refining patient selection criteria, and acknowledging the complex variables that exist within the clinical ecosystem. Ultimately, reducing variability is the key to amplifying treatment effects.
APA Citation:
Remis, A., Roundy, P., LeBlond, N., Ballay, C., Carvalho, M., & Cook, C. E. (2026). Why are treatment effects so small in musculoskeletal interventions? Part II: variability in clinical translation. Journal of Manual & Manipulative Therapy, 1-7. https://doi.org/10.1080/10669817.2026.2619675
Source: PubMed Original Article