The Challenge of Chronic Pain After Orthopedic Injury
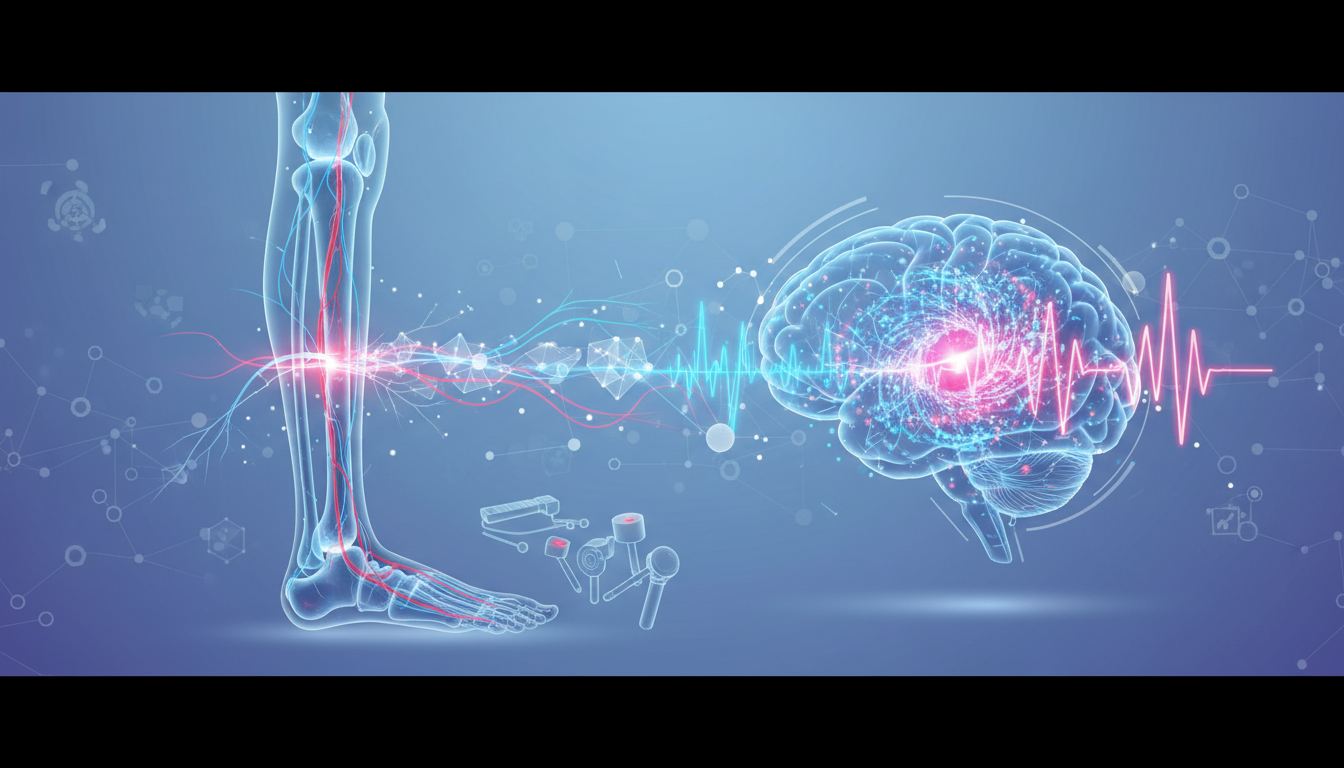
Orthopedic trauma remains a leading cause of global disability. Statistically, nearly half of individuals who undergo major orthopedic surgery for traumatic injuries will develop chronic pain, a condition that significantly impairs quality of life and increases healthcare costs. Traditional pain assessments often rely on subjective patient reporting, which can be influenced by various psychological and situational factors. To bridge this gap, researchers are investigating Quantitative Sensory Testing (QST) as a standardized, objective method to characterize pain sensitivity and identify those at high risk for chronic pain early in the recovery process.
Study Overview: Testing Feasibility in the Field
A recent longitudinal study published in the Clinical Journal of Pain examined the feasibility of using a portable QST battery in patients six weeks after major orthopedic trauma. The study, conducted across multiple sites including Johns Hopkins and Vanderbilt University, focused on 29 participants. The goal was to determine if QST procedures—specifically static measures, mechanical temporal summation, and conditioned pain modulation—could be integrated into standard post-operative clinical visits. By measuring how the nervous system processes stimuli, QST provides insight into neuroplastic changes that occur post-injury. Mechanical temporal summation, for instance, evaluates the wind-up of the central nervous system, while conditioned pain modulation assesses the body internal pain-inhibits-pain mechanisms.
Clinical Findings and Patient Tolerability
The results indicate that QST is highly acceptable to patients in the acute-to-subacute phase of recovery. Key findings from the feasibility indices include:
- 77% recruitment rate among eligible patients, showing high interest in the protocol.
- 100% tolerance: No participants withdrew due to discomfort or reported clinical pain spikes after the procedure.
- A positive association was observed between static QST measures and pain interference levels at the initial six-week mark.
- The portable nature of the testing battery makes it potentially suitable for diverse clinical environments and multi-site research.
Identifying Barriers to Implementation
While the study confirmed that patients are willing to undergo testing, several logistical hurdles were identified that must be addressed in future clinical trials. Retention remains a significant challenge, with only 57% of participants completing the six-month follow-up survey. Additionally, 38% of patients were using analgesics at the time of testing, which poses a significant barrier as medication can mask or alter sensory phenotypes. Technical difficulties also arose when attempting to apply QST to specific injury sites, particularly in patients with complex upper extremity trauma or limited access to the site of injury due to hardware or bandages.
Conclusion and Future Directions
The feasibility of QST following orthopedic trauma opens the door for a more personalized approach to pain management. By identifying specific sensory phenotypes, clinicians may eventually be able to tailor interventions to prevent the transition from acute to chronic pain. This research underscores the potential for objective biomarkers in orthopedic recovery. Moving beyond the 0-10 pain scale allows for a sophisticated understanding of a patient neural profile, which is essential for the next generation of precision medicine. While logistical barriers like medication use and long-term retention persist, the study provides a roadmap for refining these objective assessments.
APA Citation:
Aaron, R. V., Rassu, F. S., Archer, K. R., Stone, A. L., Priest, A., Bhattiprolu, K., … & Campbell, C. M. (2026). Quantitative Sensory Testing Following Orthopedic Trauma: A Longitudinal Multi-Site Feasibility Study. Clinical Journal of Pain, 10.1097/AJP.0000000000001357.
Source: PubMed Original Article