The Neural Link in Patellofemoral Pain
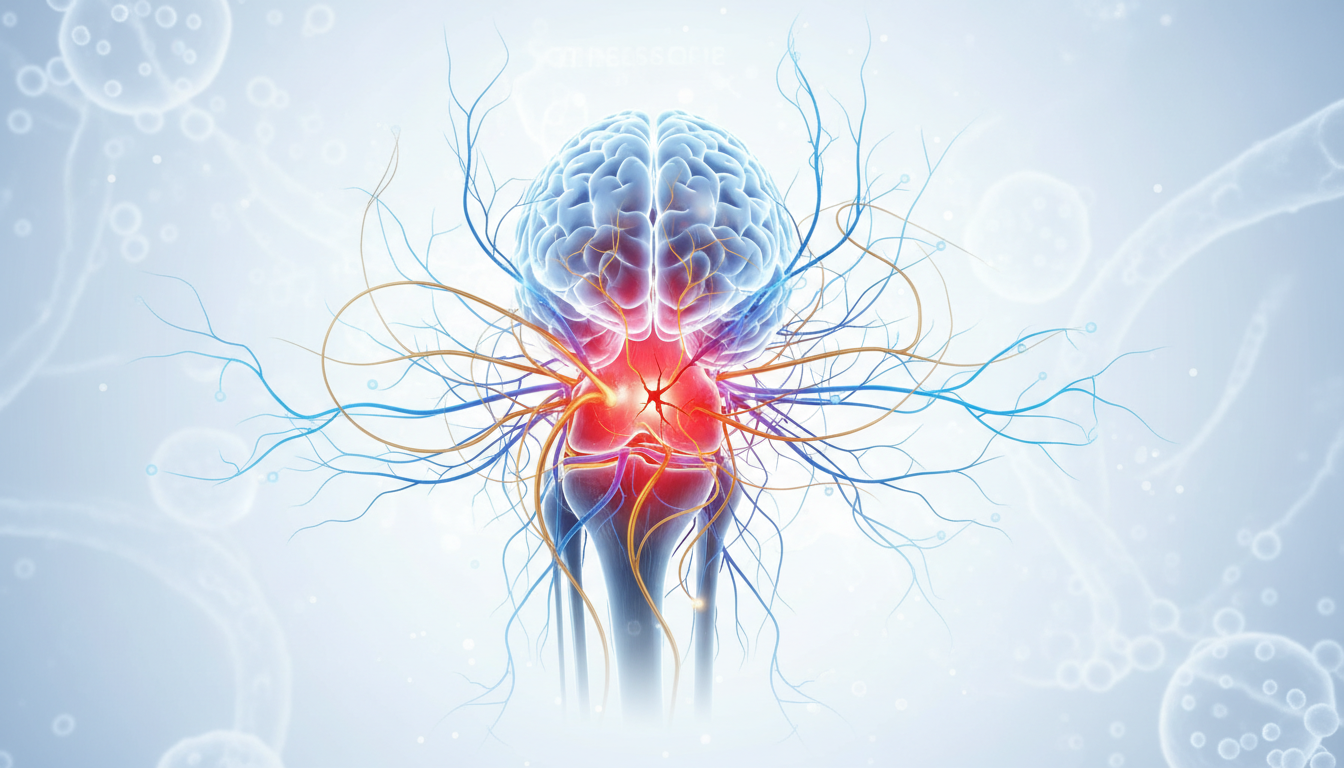
Patellofemoral pain (PFP), often referred to as runner’s knee, is one of the most prevalent musculoskeletal conditions, frequently affecting athletes and active individuals alike. While traditional rehabilitation focuses heavily on biomechanics and peripheral muscle strengthening, emerging evidence suggests that the central nervous system plays a critical role in the persistence of symptoms. A groundbreaking study published in the Journal of Sport Rehabilitation explores the relationship between corticospinal excitability and the clinical presentation of PFP, suggesting that the brain’s control over the quadriceps is significantly altered in this population.
Study Overview and Methodology
The research team, led by Gevrek Aslan et al., conducted a cross-sectional study involving 21 individuals with PFP and 21 pain-free controls. The primary objective was to investigate whether the brain’s motor cortex, specifically the pathways controlling the quadriceps, exhibits altered excitability. To assess this, researchers utilized Transcranial Magnetic Stimulation (TMS), a non-invasive technique that measures how signals travel from the motor cortex to the muscles. The methodology was comprehensive, including evaluations of:
- Resting Motor Threshold (RMT) and Active Motor Threshold (AMT): Measures of general corticospinal excitability and motor neuron membrane stability.
- Cortical Silent Period (CSP): An indicator of intracortical inhibition, reflecting the activity of GABA-B receptors in the motor cortex.
- Short-interval Intracortical Inhibition (SICI): A measure of GABA-A mediated inhibition.
- Functional Metrics: Quadriceps strength via manual muscle testing and force sense via pressure biofeedback.
Clinical Findings: Increased Cortical Inhibition
The results revealed a significant neurophysiological difference: individuals with patellofemoral pain exhibited a bilaterally longer Cortical Silent Period (CSP) compared to healthy controls. In the context of motor control, a longer CSP indicates increased inhibition within the corticospinal tract. Essentially, the ‘brakes’ in the motor cortex are applied more heavily when trying to activate the quadriceps. Importantly, this increased inhibition was not a localized phenomenon but was found bilaterally, suggesting a systemic neural adaptation rather than a purely structural knee issue. The study also highlighted several critical correlations:
- Pain Severity: Longer CSP durations were associated with higher pain intensity and longer overall pain duration.
- Functional Decline: Increased inhibition correlated with lower self-reported knee function scores on clinical scales.
- Muscle Weakness: There was a direct link between longer CSP and reduced quadriceps strength, suggesting that neural ‘noise’ or inhibition directly contributes to physical capacity.
Conclusion and Future Implications
This study provides compelling evidence that patellofemoral pain is more than just a localized knee issue; it is associated with measurable neuroplastic changes in the primary motor cortex. The findings suggest that the chronic experience of pain may lead to increased cortical inhibition, which in turn contributes to quadriceps weakness and functional limitations. For clinicians, these results underscore the potential need for ‘brain-up’ rehabilitation strategies. Integrating techniques such as neuromodulation, biofeedback, or cognitive-motor training alongside traditional exercise may be necessary to address the underlying neurophysiological barriers to recovery. Future research should focus on whether targeted interventions can reverse these cortical changes and improve clinical outcomes for those suffering from chronic PFP.
APA Citation:
Gevrek Aslan, C., Kilinc, H., Cengiz, B., Turhan, E., & Kinikli, G. I. (2026). Impaired Corticospinal Excitability of the Quadriceps in Individuals With Patellofemoral Pain is Associated With Worse Pain, Function, and Strength. Journal of Sport Rehabilitation, 1-10. https://doi.org/10.1123/jsr.2025-0012
Source: PubMed Original Article