An Aitken fracture refers to a specific type of pediatric radial neck fracture — an injury that occurs near the top of the radius bone just below the elbow joint. Named after George T. Aitken, who classified radial neck fractures in children, this fracture typically results from a fall onto an outstretched hand and often affects active children between the ages of 4 and 14 (1). These fractures are less common than other pediatric elbow injuries, such as supracondylar fractures, but require careful evaluation due to potential complications with elbow motion and growth plate involvement.
Symptoms
Children with an Aitken fracture may present with the following symptoms (2).
- Pain and tenderness over the lateral (outer) side of the elbow
- Swelling and bruising around the elbow joint
- Reduced range of motion, particularly during forearm rotation (pronation and supination)
- Inability or unwillingness to move the elbow due to pain
- A possible visible deformity, although this is uncommon in less severe cases
- Crying or distress in younger children who cannot verbally express pain
Because the injury may not appear severe on initial inspection, especially if swelling is minimal, it’s essential not to underestimate a child’s complaints of elbow pain following trauma (2).
Causes
The most common cause of an Aitken fracture is a fall onto an outstretched arm, a mechanism that transmits force from the wrist to the elbow, concentrating stress on the radial head and neck (3). Specific activities and scenarios that may lead to such injuries include
- Falling while running or playing on hard surfaces
- Sports-related accidents, particularly in gymnastics, cycling, or playground activities
- Tripping and landing awkwardly during routine play
- Direct trauma to the elbow from an object or collision
The angle at which force is applied plays a critical role. The valgus stress (a force pushing the elbow inward) is particularly likely to cause displacement at the radial neck.
Risk Factors
Certain factors can increase the likelihood of sustaining an Aitken fracture (3)
- Age: Children aged 4 to 14 are more prone due to open growth plates and increased physical activity
- Participation in high-impact or contact sports
- Inadequate protective equipment or lack of supervision during physical activities
- Previous elbow injuries that may have weakened the joint structure
- Bone health issues, such as osteogenesis imperfecta or nutritional deficiencies like low vitamin D or calcium
Diagnosis
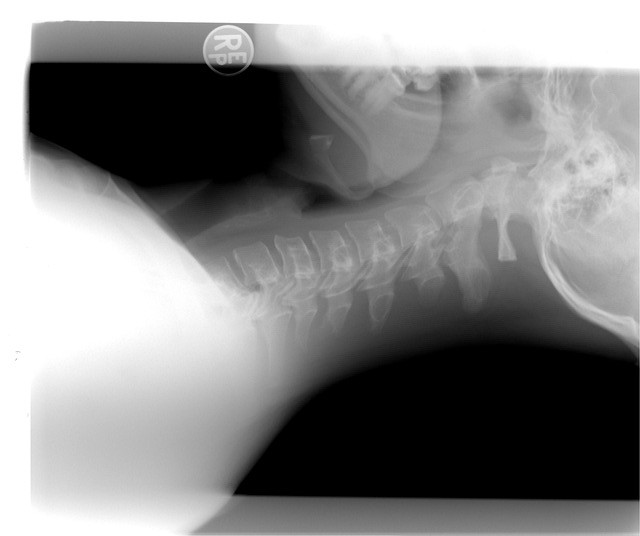
Diagnosing an Aitken fracture involves a thorough clinical examination combined with imaging studies (2).
- Physical Examination: The doctor will check for tenderness, swelling, and range of motion. The child may resist forearm rotation due to pain at the radial neck.
- X-Rays: Standard anteroposterior (AP) and lateral views of the elbow are taken. Oblique or radial head-capitellar views may be added to visualize displacement better (1).
- Aitken classified radial neck fractures into types based on angulation and displacement:
- Type I: No displacement
- Type II: Angulation <30°
- Type III: Angulation >30°
- Type IV: Severe displacement or dislocation
- Aitken classified radial neck fractures into types based on angulation and displacement:
- CT Scan or MRI (if needed): Used in complex cases where soft tissue or joint integrity must be evaluated further or if plain X-rays are inconclusive.
Treatment Options
The treatment of an Aitken fracture depends on the degree of displacement and angulation
Non-Surgical Treatment
- Immobilization: For minimally displaced or non-displaced fractures (Type I or II), a posterior long arm splint or cast is applied for 2 3 weeks.
- Pain management: NSAIDs like ibuprofen are commonly used.
- Physical therapy: Gentle range-of-motion exercises are introduced after initial immobilization to avoid stiffness.
Surgical Treatment
- Required for significantly displaced fractures (Type III or IV) or if reduction fails.
- Closed reduction with percutaneous pinning: A less invasive method where the bone is realigned without opening the skin and fixed using pins (1).
- Open reduction and internal fixation (ORIF): Performed if closed methods fail or if there’s an associated injury.
- Postoperative care: Includes immobilization followed by supervised physical therapy.
Prompt and appropriate treatment typically results in excellent outcomes, though complications like stiffness, radial head overgrowth, or avascular necrosis can occasionally occur.
Living With or Prevention
Living With
- Recovery Timeline: Most children recover fully within 6 8 weeks. Full range of motion usually returns with proper rehabilitation (3).
- Follow-up: Regular follow-up is essential to ensure the bone is healing correctly and to detect any early signs of growth disturbances.
- Activity Modification: Avoid strenuous activities or sports until cleared by a healthcare professional.
Prevention
While not all injuries are preventable, certain strategies can reduce the risk:
- Encouraging safe play practices and using protective gear during sports
- Supervising younger children, especially in playgrounds or elevated areas
- Educating children about fall safety
- Maintaining bone health through adequate calcium, vitamin D, and physical activity
In cases where a child has sustained a prior fracture, addressing any underlying bone weakness or coordination issues may be helpful.
References
- Langenberg LC, van den Ende KIM, Reijman M, Boersen GJJ, Colaris JW. Pediatric Radial Neck Fractures: A Systematic Review Regarding the Influence of Fracture Treatment on Elbow Function. Children (Basel). 2022 Jul 14;9(7):1049. doi: 10.3390/children9071049. PMID: 35884033; PMCID: PMC9324597.
- De Mattos CB, Ramski DE, Kushare IV, Angsanuntsukh C, Flynn JM. Radial Neck Fractures in Children and Adolescents: An Examination of Operative and Nonoperative Treatment and Outcomes. J Pediatr Orthop. 2016 Jan;36(1):6-12. doi: 10.1097/BPO.0000000000000387. PMID: 25812145.
- Lewallen L, Elliott ME, McIntosh A, Ho CA. Pediatric Elbow Dislocations and Associated Fractures. Children (Basel). 2023 Jun 1;10(6):993. doi: 10.3390/children10060993. PMID: 37371225; PMCID: PMC10297433.